There’s lots of dangers inherent in trail running, risks we all accept as part of the experience of going wild. One of them potentially prevalent across many trail running nations can leave runners bedridden, yet you won’t see the accused culprit coming. US-based Murray Susser, MD, gives oversight to the problem of ticks and the particularly nasty disease they can infect you with.
[NOTE: it has been pointed out to TRM that in Australia there is, according to the Australian Government and its health officials, no conclusive proof that Lyme Disease-like symptoms presenting in some patients are actually caused by tick bites or the bacteria that is known to cause Lyme-disease in other nations. Thus the existence of Lyme in Australia is contentious and not to date proven. The most recent media statement from the AU government can be read here and a general page on Lyme disease status from official quarters here. The opinions and judgements in the article below are those of the author, not necessarily those of TRM, but we’re open to the debate… And it still pays to be careful when running in those nations where Lyme Disease is 100% confirmed.]
It was supposed to be an ‘easy’ 6-hour 1-minute, 50-mile (80km) race, back in 1990. Two days later, Bart Yasso, ‘Chief Running Officer’ at Runner’s World magazine had a headache and fever. He thought the race wore him out. A “bull’s-eye” rash appeared giving some indication this wasn’t just a case of extended post run fatigue. After three weeks of aching joints, Yasso couldn’t run a 10-minute mile. Something was wrong.

Bart Yasso during one of his many trail races.
It wasn’t to be the last time the author of My Life on the Run was to contract Lyme Disease, a bacterium passed on to humans by tick bites and something trail runners can be particularly at risk of given their love of running in the wilderness. Although Yasso warns: “Trail runners think I was in the middle of nowhere when I was bit, but they don’t realize a tick can attach in the grass of a parking lot.”
Come 1997 and the symptoms were back in force.
“It was 100 times worse,” Yasso says.
Yasso went to Africa to climb Mount Kilimanjaro. He didn’t make it. He ended up in a Tanzanian hospital where doctors thought he was going to die. They didn’t know how to treat him, so he flew back to the states.
Yasso received six months of intravenous antibiotic treatment and went into remission. In 2002, while in his 40s, he finished second overall in a 50km race.
Another accomplished trail runner, Dylan Armajani, founder of Trail Whipp Ass (www.trailwhippass.com), was diagnosed with Lyme last July 2014. After volunteering for the NY/NJ Trail Conference he saw a blood-filled tick on his leg, but he couldn’t find a bite mark. Two weeks later he saw red rashes on his leg. He went to an ILADS (International Lyme And Associated Diseases Society) expert in New York City and was treated and is now in remission.
Some trail runners known to Yasso haven’t treated their tick bites with enough caution or prompt treatment, he believes.
“’It’s no big deal,’ they’d quip and start running too soon. When I saw them six months later, they could hardly get out of bed.”
Even today, when Yasso pushes himself, his legs and joints swell.
Prevention is better than treatment, but once you contract the disease, receiving the correct treatment from a Lyme expert is vital.
Almost every working day I treat people with Lyme disease. I’ve seen the gamut of reactions, from mild to severe. My interactions have mostly been with patients after they contracted Lyme or the co-infections.

Gary Scarano after finishing the Hook Mountain Half Marathon Credit: Wojciech “VT” Cieszkowski
One of my staff, Gary Scarano, is a trail runner and believes runners tend to have a cavalier attitude about the disease. This year alone, three of his friends contracted Lyme disease.
“Many runners don’t know or don’t worry about Lyme prevention or treatment,” he says. “They believe prevention is ‘pulling ticks off after a run’ and if they contract the disease, a quick trip to the doctor’s for antibiotics will suffice.”
Both assumptions could be wrong.
Dr. Susser’s Lyme Disease Tips for Trail Runners
Lyme Disease is named after the town of Lyme, CT where it became recognised as an issue in 1975. It’s caused by a bacterium called Borrelia burgdorfori. This spirochetal (corkscrew shaped) organism reaches the human body through a tick bite after it has bitten an infected white-footed mouse or deer, and gets the Borrelia in its blood. The infected human then suffers, at first, a flu-like illness with fever, chills, headache, muscle pain, malaise, and fatigue. If the immune system fails to stop it, it progresses on to multi-system disease, including arthritis, and neurologic, and cardiac disease.
There has been speculation Lyme can be transmitted in other ways (e.g. blood transfusions or other insects), but this has not been proven.
Danger zones
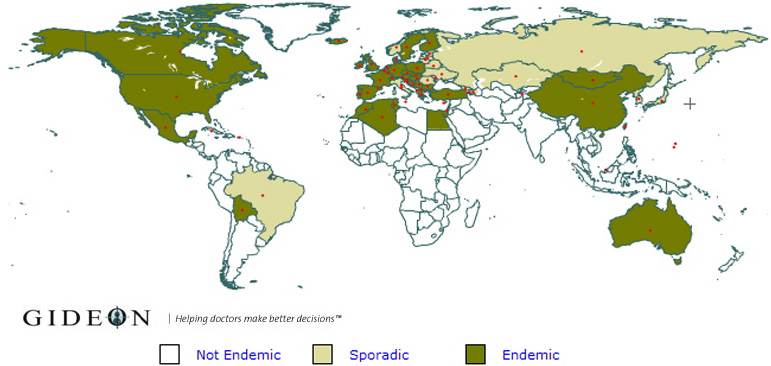
Lyme Disease is considered endemic in North America, much of Europe including the UK, parts of northern Africa, China, Mongolia, southern Chile and Bolivia. It is also sporadic across Russia and Eastern Europe and Brazil.
Prevention
- Runners should cover arms, legs, and wear a hat making it harder for ticks to attach.
- Remove your shoes and outer layer of clothes, shake them, and leave them outside.
- Complete a tick check and shower immediately. Brush the surface of your skin away from your body.
- If you find a tick attached to you, take tweezers and grab it, but don’t squeeze it, to remove. Preserve the tick in your freezer for later testing.
Treatment
- Treat it aggressively.
- See a Lyme specialist doctor and explain you want to continue running.
- Ration your energy. Your immune system needs it to fight infection.
Remission
The Lyme organism Borrelia, can take the form of a cystic which can be dormant for years. It can come back, usually after some strain or stress. For example, people who have taken steroid drugs, which weakens the immune system, could trigger a reoccurrence. Having Lyme does not give you immunity. Once you have it, it could come out of remission.
[ED’s NOTE: for the status of Lyme Disease in Australia, according to the Australian Government, please see information here. ]
 Murray Susser, MD, is a Lyme disease expert and has been treating Lyme for decades. He co-wrote the book Solving the Puzzle of Chronic Fatigue Syndrome. He believes a key piece to this puzzle is Lyme disease. Dr. Susser’s website is www.MurraySusserMD.com.
Murray Susser, MD, is a Lyme disease expert and has been treating Lyme for decades. He co-wrote the book Solving the Puzzle of Chronic Fatigue Syndrome. He believes a key piece to this puzzle is Lyme disease. Dr. Susser’s website is www.MurraySusserMD.com.